Breastfeeding is an emotive issue . Everyone has an opinion on whether breastfeeding is best and whether formula feeding is ever as good. Mothers who breastfeed are judged , mothers who formula feed are vilified. There are social, behavioural, cultural, religious and medical factors that weigh in on how you perceive what is best for your baby. For any new parent, navigating the sea of opinion and unsolicited advice can be very difficult, without having to consider HIV. When we add HIV to the mix, the judgments amplify and fear dictates decisions.
In my practice, I work with a number of couples from pre-conception all the way to infant HIV care. It's one of my favourite things to talk about because I am passionate about it. I have two children, one who was breastfed and one who was formula fed. I know first hand how difficult it can be to establish breastfeeding and how little support there is out there for breastfeeding mothers. It means a lot to me that my patients are offered support in this decision, and that they have no regrets 2 years down the line.
Many Obstetricians, GPs, Paediatricians and midwives advise against breastfeeding because the "risk is too high". But are all these specialists able to quantify or qualify what the actual risk of HIV transmission is? It is unacceptable to me that this coercive approach is taken instead of offering full information, including the pros and cons. We call this informed decision making.
Why are people afraid to Breastfeed if HIV positive?
In short: because they wish to eliminate risk.
- the HYPE
- HIV stigma has resulted in increased ignorance, fear mongering and decreased tolerance.
- There is a general belief out there that if a mother is HIV positive, then the baby will be born with HIV. This is false.
- There is a belief that the risk from Breastfeeding is "HIGH" and therefore unacceptable. Medical professionals, including HIV specialists, amplify the risk without quantifying it. Most countries guidelines state that formula feeding should be offered to higher socio-economic groups and breastfeeding used in low income settings. These guidelines not only ignore the biological drive of a mother to breastfeed, but also enforce the stigmatisation of it. It smacks of the old paternalistic medical practice we have moved away from and undermines a natural process.
- In the absence of any interventions, the risk of MTCT is approximately 30%–40%. (But with interventions, the risk is <1 b="">)
- the HISTORY
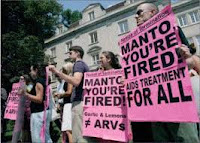
- The South African government provided free formula for 6 months to all HIV positive mothers from 2004 to 2010. Women were advised against breastfeeding but it was thinly disguised as "counselling"
- (Women were told "Mummy, if you breastfeed then the baby can get HIV. So, what will you choose? " )
- Then pivotal studies like the Mashi study, Kesho Bora , BAN and others showed that HIV exposed babies were still as likely to die by the age of 2 regardless of whether they breastfed or formula fed. The difference was that the Breastfed babies were dying from HIV while the formula fed babies were dying from infectious diseases (like gastroenteritis, pneumonia and malnutrition). They also showed that providing ARV treatment to the mothers and Post Exposure Prophylaxis to the infants, proffered significant protection against HIV transmission.
- As a Result of this, WHO revised its recommendations in 2010 to advocate for breastfeeding in HIV positive mothers.
- the wish to do no HARM
- Health professionals honestly have the intent to help and to do No HARM. However, sometimes, in their eagerness to prevent harm (by recommending against breastfeeding) they inadvertently do Not DO good (by stripping the mother of her right to choose, by not providing her with an informed decision making process, and by ignoring the potential disadvantages of formula milk)
- Mothers are desperate to protect their child and are also ill informed. There is emotional blackmail and recommendation to avoid breastfeeding with an implication that she is doing something negligent by offering her baby breast milk.
What is the risk of HIV transmission through breastfeeding?
To understand the risk better it is necessary to look at a study. The study below really highlights the pertinent issues. Skip the images if you can't bear the detail, but read the text.
Mary Ngoma et al (study published July 2015)
In this study 279 Women were also given ARVs while pregnant. All were encouraged to Exclusively Breastfeed for 6 months. From 6 m to 12 months age, they breastfed and gave complementary foods. They stopped breastfeeding 13 months. The table below shows that
after 6 weeks NO infant had acquired HIV through breastfeeding!
after 6 weeks NO infant had acquired HIV through breastfeeding!
And interestingly, after 12 months there were 3 infected babies. But, each case was linked to a high viral load in the mother. This means that after a year, if the mother demonstrated successful ARV treatment with a low viral load, there were no children infected with HIV. ( see image below)
It is a gold standard to promote exclusive feeding, but did this really happen in these mother infant pairs? At no single point in time were all the mothers exclusively breastfeeding. (see graph below)
- 98% of mothers were Exclusively Breastfeeding while 2% of mothers were mixed feeding from birth
- by 1.5 months this had dropped to 95% breastfeeding exclusively and 5% of infants were mixed fed and
- by 3 months a further drop to 92% exclusive while 8% of infants were mixed fed or had started formula.
- Between 3 and 6 months the exclusive breastfeeding dropped from 92% to 15% ! At 6 months only 15 % of infants were being exclusively fed. That is a very low percentage. This tells us that most infants have other food introduced before 6 months despite WHO recommendations. Which tells us that the WHO recommendations are not pragmatic and not practicable.
Definitions
Exclusive Breast Feeding
Only Breast milk (either expressed or directly from the breast but definitely breast milk) is given. No water, No formula top ups, no porridge and no solids given. This is recommended by the World Health Organisation for the first 6 months of life. (However, it is also important to note that there is flexibility between 4 and 6 months of age to assess whether the infant is now ready to add additional foods other than breast milk)
Only Breast milk (either expressed or directly from the breast but definitely breast milk) is given. No water, No formula top ups, no porridge and no solids given. This is recommended by the World Health Organisation for the first 6 months of life. (However, it is also important to note that there is flexibility between 4 and 6 months of age to assess whether the infant is now ready to add additional foods other than breast milk)
Complementary Feeding
When breast/formula milk is still given but it is now age appropriate to add in additional foods, like vegetables, solids, tea, water. Age appropriate refers to the infants gut maturity and its ability to now safely digest different foods of different textures and other contents. It also means that the infants brain has developed sufficiently to coordinate chewing and swallowing. It is a natural progression because milk alone is no longer sufficient to provide all the infants nutritional needs.
Mixed Feeding
Mixed Feeding is Inappropriately including foods other than Breast Milk (or Formula Milk ) at a time when the infant's gut is not mature enough to be able to digest these foods. Commonly, in South Africa, cereals get introduced within the first few weeks of life. These foods have a much coarser texture and can cause microscopic tears in the gut. These food may also trigger an immune response in the infants gut that makes the infant more susceptible to illness, allergy and later metabolic conditions. It is important to understand the difference between Mixed and Complementary feeding. What does this study is tell us?
When mothers were treated with ARVs effectively to a viral load less than 1000 copies/ml then there were NO HIV infections. AND, most mothers introduced other foods before 6 months but no infections occurred. Pretty cool neh?
No one can ever give you a guarantee that your baby will be HIV negative. But taking ARVs gets you as close as is humanly possible to eliminating risk to the baby.
Breastfeeding can offer a phenomenal amount of benefit to baby, and to mum. My agenda is to ensure that the word gets out, and to ensure that mothers get a Choice. A choice to take ARVs, a choice in how they deliver the baby, and to choose how they feed their precious child.










There is another great option to cure herpes, with herpes home remedy. It is simply because so many of us don't know the right one to meet at the right time . I was deadly in pain of herpes for six months, I tried different cure but it could not heal, one day my friend Jane saw a testimony of a lady'Edith' on this blog. how her herpes was cure by Dr Akhigbe with his herbal medicine cure that can help to heal the blister and sores of herpes totally.We write to him through his email, drrealakhigbe@gmail.com he told us that he was going to help us. He prepared the medicine and sent it to us through UPS courier services , he also instructed me on how i will be drinking the herbal medicine for three weeks. My dear brothers and sisters, Dr Akhigbe herbal medicine cure is real and it cure my herpes totally. So i must testify of him, he is a good man and i call him daddy.. If there any one out there that need his help because Dr Akhigbe cure different diseases.. Please contact him on his email... drrealakhigbe@gmail.com or you can also whatApp him with these number +2348142454860 Dr Akhigbe is good herbalist man to be trust.
ReplyDelete